Welcome to On The Mind, a collection of stories, news, and analyses on the startups, investors, and thought leaders in mental health and wellness.
Here’s what’s included in issue No. 7:
Turnkey solution integrating behavioral health with primary care visits
Overview of the Collaborative Care Model, and why it works
YouTube entertainment that offers an antidote to dissatisfaction
🎙️ Interview with Spencer Hutchins, CEO of Concert Health
Conversations with founders, investors, and thought leaders in mental health and wellness.
Spencer Hutchins worked through a mix of jobs spanning politics, consulting, and technology before founding Concert Health in 2016. San Diego-based Concert Health helps independent physician practices deliver integrated behavioral health services to their patients, including care management, brief therapy interventions, and psychiatric consultations. Today, Concert operates across 8 states and partners with over 40 medical groups, from large-scale organizations including CommonSpirit Health and Women’s Health USA to smaller, independent practices. The company has cared for over 10,000 patients.
Spencer and I spoke this week about his professional journey, how he built Concert, and what’s next for the future of mental health in primary care.
I was excited to see you used to work at Booz & Company, my former employer. We didn’t overlap, but how did you go from consulting to entrepreneurship?
Yeah - well, I’ll start from the beginning. I kicked off with political campaign work out of college, working on John Kerry’s Presidential campaign. I ended up going to business school because I wanted to bridge the public and private sectors into my career - I wanted something that was public-spirited but I had a passion for big organizations and their ability to make a difference at scale. After school I landed my consulting gig, and spent half of my time working with healthcare clients and the other half with technology clients.
I took a sabbatical from work in 2009 to join the first term in Obama’s administration, working for the first healthcare group at the FCC. This was when iPhones were still relatively new and nobody understood their impact on our health - the FCC regulates phones in the same way the FDA regulates healthcare, and I was at the intersection of new territory.
After the sabbatical I returned to consulting but quickly realized I wasn’t hard wired to be an advisor. I had an opportunity to come out to San Diego to work for a friend in an investing role, but ultimately found that was similar to working as a consultant, just with more teeth.
I wanted to be operating, building, doing. I founded my first company, Reflexion Health, a software business that provided an FDA-cleared solution to support physical therapy from home. I ran that business for several years, and eventually sold it in search of my next adventure.
I had no background in behavioral health, but professionally I had spent 10 years adjacent to it and saw it as a segment that was underinvested in, broken, and ripe for optimization. I had close friends and family who had personally experienced how transformative good behavioral healthcare could be. I came across the Collaborative Care Model, ultimately became convinced of its effectiveness, and decided to build Concert Health around it.
What was so convincing about the Collaborative Care Model?
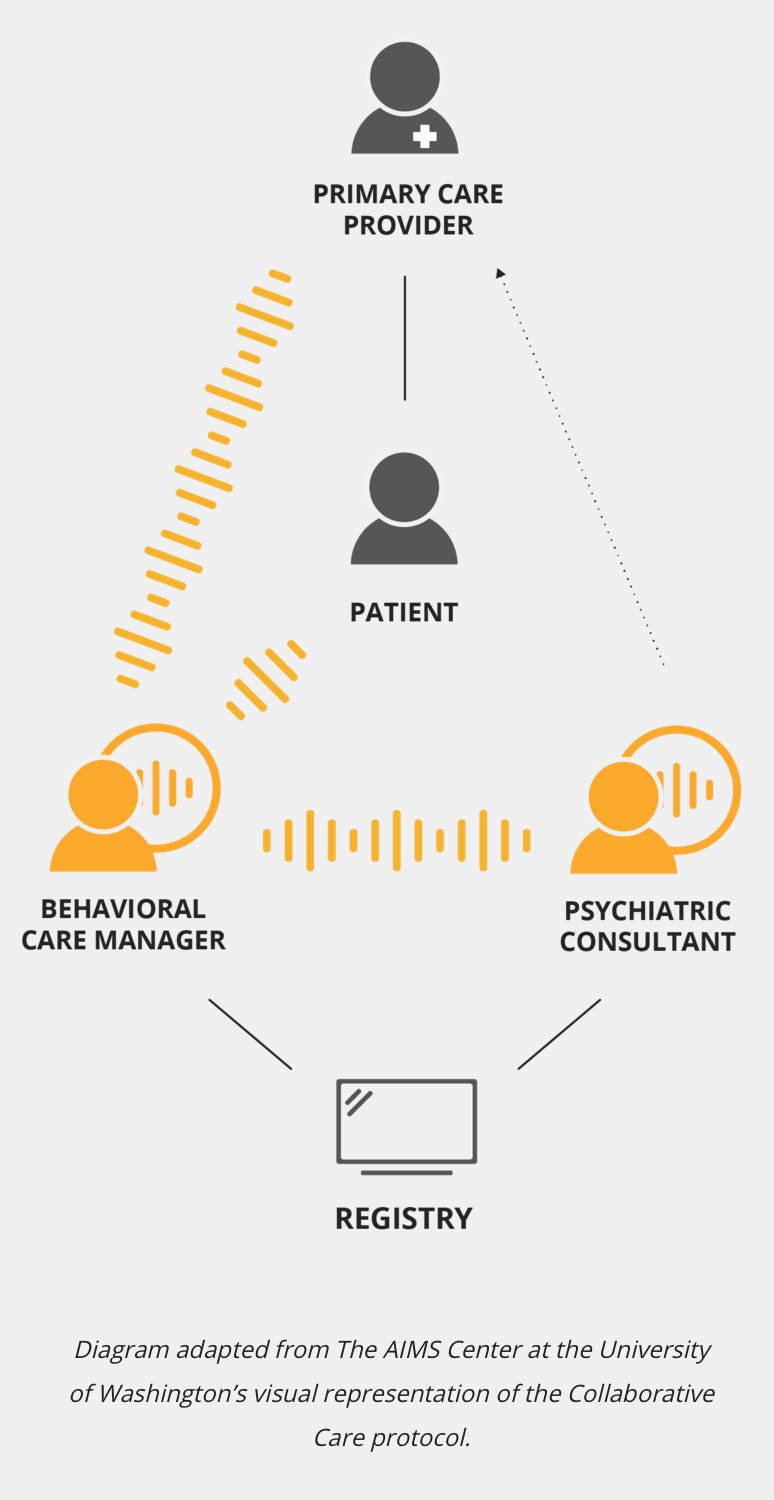
The Collaborative Care Model is all about integrating behavioral health into the primary care setting. It combines the work of three care team members: a primary care provider (PCP), behavioral care manager, and a psychiatric consultant. The model is always evaluating symptom severity, trying interventions, and if those don’t work, trying new ones.
I was convinced by the enormous amount of research around it. There are over 80 randomized controlled trials (RCTs) that prove its efficacy. When starting a business, you could pursue new science, such as the biotech industry does, or you could scale existing science, which is what we did. Instead of needing to prove something new, we just had to figure out why the process, technology, or business model hadn’t yet worked.
I teamed up with my Co-Founder Virna Little, a psychologist and social worker herself - she saw the same opportunity, started as an advisor, and then came on full-time as COO.
If it’s such a good model, why weren’t others already implementing it?
The problem was not the model itself; the model was already being implemented. There had been huge amounts of grant-funded research, and capitated systems like Kaiser had been early adopters of the model. It was a matter of nobody figuring out how to scale it successfully.
The first reason it was difficult to scale came down to money. As much as some teams tried to do behavioral health and primary care integration, the financial incentives weren’t in place - behavioral health specialists and PCPs got paid differently and patients would pursue the services and price points that worked for them, whether or not they were connected. We came in at the right place and time, when Medicare just began making the Collaborative Care Model a covered benefit, helping to shift the payment dynamics and set the foundation for the model to work.
The second reason nobody did this at scale was just the pure complexity of it all. When we talk about integration, it’s not just putting a behavioral health professional next to a PCP. It’s the patient screening, the warm handoffs, finding great clinicians, training them properly, providing the right technology and workflow. It’s not easy, and Concert was built to simplify it.
So help me understand how Concert has done that - what does the actual product look like? Can you walk me through the experience for a patient?
We operate a behavioral health medical group. The vast majority of our 130+ employees are clinicians (behavioral care managers, physicatrists, NPs). We partner with groups that serve as the key point of care for patients - typically primary care groups or women’s health groups - and deliver care together. Today, our teams mostly work from home, but we’ll likely revert to a co-location model post-Covid.
In a standard PCP office visit, a patient may bring up feelings of depression or anxiety in the 6th minute of a 7 minute visit (if they even bring it up at all - over 50% of patients won’t say anything). The PCP may write a prescription, encourage them to look for a therapist, and then send them on their way.
The offices we work with have entirely different processes, starting off with a much better job at screening. When a PCP walks into the office, she’ll know if the patient scored positive on their PHQ-9 or GAD-7. She’ll be trained on the right language to use - careful to focus on symptoms like sleep issues or energy deficiencies, suggesting that a “care manager” can provide additional support where needed rather than forcing the words “behavioral health specialist” or “therapist,” which can be offputting for some. After the PCP visit, the patient will receive a follow-up from the behavioral health care manager, who can provide a spectrum of interventions, depending on individual needs. It could be something more involved such as outpatient therapy, or something much milder like light-touch check-ins or symptom monitoring.
The PCP herself will be in continuous communication with the behavioral care manager, and will speak with a psychiatric consultant on a weekly basis to discuss certain patients. The psychiatrist doesn’t take over the care, and is not a referral from the PCP - rather, she and the PCP jointly consult with the care manager to determine the appropriate interventions. We’ve been really focused on delivering fidelity to this model and making it as strong as possible.
How have things improved over time?
We’ve continued to evolve and extend the model with a focus on clinical excellence, largely due to Virna’s leadership.
One huge improvement for us has been a real focus on suicide-safer care. The 9th question on the PHQ-9 is around whether you have thoughts of hurting yourself or others. For those who answer positively, there’s another scale called the Columbia-Suicide Severity Rating Scale (C-SSRS) - this helps assess where patients fit along that continuum. We’ve done a lot to create a structured safety plan so that the most vulnerable patients are properly tracked and cared for. In addition to a depression and anxiety registry, we also have a suicidality registry, which we can prioritize for more frequent check-ins or emergency interventions with patients as needed. The standard answer for handling suicide risk is sending people to the emergency room, but this can be ineffective and cause other problems - our approach focuses on training the full care team on how to handle these situations under the thesis of collaborative care. We instill a rigorous engineering mindset around patient tracking and evidence-based intervention.
How has your customer base changed as you’ve grown?
The model itself has always been centered around integrating behavioral health into primary care. PCPs are already writing the majority of antidepressant prescriptions, so the integration has to happen there - but what constitutes primary care has shifted.
In addition to growing our core base of PCPs, we’re seeing huge growth in pediatrics practices and OBGYNs. A lot of specialists are beginning to recognize that they’re the principal physician for their patients. Most women are only connected with a gynecologist. We’re seeing this in oncology too, where cancer patients end up relying on their oncologist as their principal physician and have them take over their prescriptions and general care more broadly.
Let’s shift gears to your fundraising journey. You announced your $14M Series A at the end of January. How have you used the funds and what has your experience been like working with investors?
Securing funding has allowed us to expand from 4 to 8 states in the past few months. We continue to build out our technology team. We’ve always centered on the clinicians and invested in training and upskilling - our care managers and psychiatrists are the core of what we do, the rest of us just work for them. We’ve also made our first sales hire and are starting to ramp that up. The money from our last raise will last us a long time.
Our experience with investors has been great - we really have a wide spectrum of people backing us. Healthy Ventures led our Seed round - Anya Schiess was our first Board member and has been a great advisor. At first when you’re raising you just want money and customer intros, but once you get deeper, you want sounding boards, someone to call you out on your BS - Anya’s been doing that for years.
Town Hall Ventures has also been great. A relatively new fund, but these guys - Andy Slavitt, Trevor Price, David Mishkin - there’s nobody that knows more about large health systems or Medicare/Medicaid. Their ability to understand the trends in this space is unmatched.
Vertical Venture Partners, who led our Series A, has been the least specific to health. They do some health but focus more on general B2B SaaS models. They’re extremeley saavy about how to scale and run a commercial business and add a ton of value there.
And then there’s our individual investors like Edward Bergmark, who founded Optum. He’s someone who was at the forefront of mental health call centers at their genesis, and truly understands the potential of what we’re doing.
Sounds like a lot of exciting growth. Are you hiring for any roles right now?
First and foremost, we’re hiring an enormous number of clinicians. People who are licensed behavioral health providers, licensed psychiatric NPs - we've been bringing on 15-20 per month to keep up with demand.
We’re hiring for an experienced revenue cycle management role which we just posted, and also a couple of engineering and product roles.
Concert Health is in growth mode, so if you have a passion for what we’re doing but don’t see a specific job description that fits, send in an application anyways.
[Check our the Concert Health job board here.]
🩺 Clinical Coverage
Discussion of clinical concepts, studies, or perspectives on mental health and wellbeing.
Concert Health is built off the clinically-validated Collaborative Care Model, which is published by the American Psychiatric Association and not exclusive to the company.
The model is not new, either - this academic brief from 2013 quotes over 70 RCTs that have shown collaborative care for common mental disorders such as depression to be more effective and cost-effective than usual care, across diverse practice settings and patient populations. And that number has only grown since.
The logic behind the model is simple. Since so many still rely on their primary care provider as their core source of healthcare, it makes sense to integrate mental health services within that structure. The simple video below provides an overview of how it works:
💰 Recent Investments and IPOs
Rundown of recent investment news in mental health and wellness companies.
Atai Life Sciences, the powerhouse German startup building a portfolio of psychedelics companies, raised a $157M Series D at a $2B valuation, making it the largest psychedelics company by market cap on the planet (Link)
Behavidence, a creator of digital phenotyping for mental health, raised an undisclosed sum in its Pre-Seed round led by Fusion LA and GoAhead Ventures (Link)
BetterUp, an employee wellness startup, raised $125M at a $1.73B valuation in its Series D round led by Iconiq Growth, with participation from Lightspeed Venture Partners, Threshold Ventures, Plus Capital, Salesforce Ventures, Sapphire Ventures, and Mubadala Capital (Link)
Bionaut Labs, which uses a precision medicine treatment modality for CNS disorders, came out of stealth with $20M in financing led by Khosla Ventures (Link)
BurnAlong, a corporate wellness platform, raised a $7M Series A led by Triventures (Link)
ClinSpec Diagnostics, which has developed a spectroscopic liquid biopsy test that incorporates machine learning to detect brain cancer in just ten minutes, has raised nearly $5M (Link)
Frog Systems, a Glasgow-based online mental wellness platform, raised ~$700K led by Aldridge (Link)
Heading Health, a psychiatric clinic platform, raised an $850K Pre-Seed round (Link)
HelloSelf, a London-based AI-powered therapy service, raised ~$7.6M in a Series A led by OMERS Ventures (Link)
Limbix, a developer of a prescription digital therapeutic for the treatment of adolescent mental health disorders, was awarded a $3.6M grant from the NIMH (Link)
Pear Therapeutics, a leader in prescription digital therapeutics, announced the second closing of its Series D financing, bringing its total funding amount to $100M (Link)
Wysa, an Indian mental health AI-powered app, has raised an undisclosed sum from the Google Assistant fund (Link)
📖 Interesting Reads
Sometimes mental health-related. Sometimes just things I find interesting.
I now know way more about Excel than I ever intended to (Link)
This artificial ski slope on the top of a Copenhagen plant looks super fun (Link)
If you don’t know who Beeple is, it’s time to find out (Link)
Catch up with what’s happening with NFTs (Link)
I’m trying to stop talking about NFTs, but Elon keeps tweeting (Link)
The Atlantic is apparently bold enough to put a timeline against ‘back to normal’ (Link)
Is there really no such thing as bad publicity? McKinsey begs to differ (Link)
A counterintuitive approach to improving mental health (Link)
Database of companies applying GPT-3 across new use cases (Link)
I’m not sure why this short documentary was made, but I’m glad it was (Link)
The NYT does a deep dive into celebrity ‘ghost kitchens’ (Link)
Tips on how to use sound to shift your state of mind (Link)
Surfing in the freezing-cold Great Lakes (Link)
Female innovators leading the way in mental health (Link)
Current Affairs takes on corporate mindfulness programs (Link)
The American Psychological Association released its latest Stress in America report; the results are, unsurprisingly, not great (Link)
Could group therapy get a boost from psychedelics? (Link)
🧠 Mindfulness Tip of the Week
Tips to improve your mental health and wellbeing.
I fell down a Kurzgesagt – In a Nutshell rabbit hole this past week - I forgot how great these videos are.
The popular YouTube channel covers a variety of thought-provoking topics - it’s an easy place to go to find something to learn or entertain yourself with when you have an extra 10 minutes in your day.
Watching any of the videos can provide a nice mental break, but there are several that explicitly cover the mind in some capacity, which can be even better for practicing mindfulness. The below example is an awesome reminder of how to use gratitude as an antidote to dissatisfaction. You can’t help but feel a little more optimistic after watching.
On Your Mind
I’d love your feedback - feel free to email me at tarockoff@berkeley.edu.
If you’re working on something in mental health and wellness, let’s talk. You can book some time with me here.
Know someone who’d enjoy On The Mind?
Was this newsletter forwarded to you?
Written by Daniel Tarockoff, an MBA student at UC Berkeley and former healthcare strategy consultant exploring the future of mental health. Born in Michigan. Based in Berkeley, CA.








This article is really informative